Tara Becker is a CHIS senior public administration analyst and author of a new policy brief that analyzes the latest health insurance trends in California. In this interview, Becker discusses changes in employer-sponsored insurance (ESI) and the effects of actual and potential federal policy changes regarding elements of the ACA.
Q: ESI enrollment hit a low of 48.2 percent in 2016. But this year the rate rebounded to 51.2 percent. Meanwhile, Medi-Cal's steadily-rising enrollment rate declined from 33 percent in 2016 to 29 percent in 2017. What does that suggest to you?
Enrollment in employer-sponsored insurance coverage improved as the economy continued to improve. During this period, more Californians entered the labor force and fewer were unemployed. These changes lead to an increase in the rate of employer-provided coverage both because Californians are more likely to be working, and in a tight labor market, employers are more likely to offer health insurance coverage to attract and retain employees.
Q: The individual mandate feature of the ACA will be eliminated in January. What effect will that have on insurance rates?
The purpose of the individual mandate was to encourage younger and healthier people to purchase insurance so that the pool of Californians with health insurance coverage would have lower average health care costs. This in turn would lower health insurance premiums and make health insurance more affordable for those who have higher medical costs.
Without this incentive to purchase health insurance coverage, many younger and healthier people might opt out of purchasing insurance because their expected medical costs are lower than the cost of insurance coverage. This may reduce the pool of insured Californians primarily to those who are older and less healthy, meaning the average medical costs incurred by each individual in the pool will increase, leading to higher health insurance premiums. This may discourage even more young healthy Californians from purchasing coverage, further increasing the average costs for those who remain insured, and in an extreme case, leading to an insurance market death spiral.
In the long-term, this will make health coverage more expensive for these younger and healthier Californians when they do need to purchase health insurance in the future.
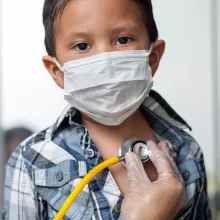
Q: Although Medi-Cal enrollment dropped in 2017, 29 percent of nonelderly Californians are covered by the state health program for low-income and disabled Californians. Which groups stand to lose most if the federal government tightens Medi-Cal funding?
Low-income Californians are the most likely to lose coverage if changes to Medi-Cal are made. In 2017, more than 60 percent of nonelderly Californians with family incomes below 139 percent of the federal poverty guidelines (FPG) were insured through Medi-Cal, as were more than 40 percent of those with family incomes between 139 percent and 200 percent FPG. Because more than 40 percent of Latinos and 30 percent of African-Americans are covered through Medi-Cal, the uninsured rate will likely rise for these groups if Medi-Cal eligibility is restricted.
Regionally, any restrictions on Medi-Cal eligibility would hit the San Joaquin Valley the hardest, because more than 40 percent of residents in this region are enrolled in the program. Both Los Angeles County (34 percent enrolled) and the Northern and Sierra counties (31 percent enrolled) also experience high rates of Medi-Cal enrollment and would likely experience an increase in the number of uninsured.