Menu - Breast Cancer
1 in 8 women will develop breast cancer in their lifetime.
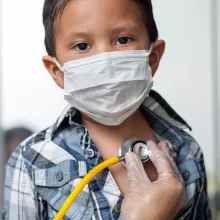
In the past decade, UCLA Center for Health Policy Research researchers have focused on the barriers women with breast cancer face, and how policy solutions can help break them down. For patients with breast cancer, access to care is often stymied by lack of money, insurance, or information about new kinds of testing and treatment, as well as language and cultural differences that require health care navigators.
Examples of our breast cancer research:
In 2021, UCLA researchers from the UCLA Center for Health Policy Research and the UCLA Jonsson Comprehensive Cancer Center published recommendations for California policymakers and patient advocates aimed at improving care and outcomes for women with metastatic breast cancer (MBC), based on a 2020 report, Barriers to Metastatic Breast Cancer Care in California: A Report to the California Breast Cancer Research Program. The report made three critical recommendations that were based on caretaker and patient interviews:
- Removing health insurance obstacles;
- Improving participation in clinical trials; and
- Increasing access to palliative care.
Fact sheets related to each recommendation were published in English, Spanish, and Chinese.
Researchers also conducted a qualitative study on how a Twitter “chat” with the MBC community helped identify barriers and policy solutions for care.
Breast Cancer Social Media (#BCSM) Twitter Chat at a Glance
288
tweets
42
users
2.1 million
impressions
In 2018, UCLA CHPR researchers released the report Addressing Barriers to Breast Cancer Care in California: The 2016–2017 Landscape for Policy Change and discussed findings at a legislative briefing in Sacramento, along with State Senator Richard Pan and cancer survivor Veronica Vera. Three related fact sheets released the day of the briefing focused on primary issues of narrow networks, timely care, and cultural barriers.
In 2015, a UCLA CHPR study reported that 1 in 5 women were unaware of a test that could predict whether there was a greater chance for their breast cancer to return which would influence whether or not having chemotherapy had value.
Additionally, the California Health Interview Survey (CHIS) has included questions about cancer prevalence and whether Californians receive preventive screenings — lung, breast, colon, prostate, cervical — for cancer, or vaccines to prevent cancer, such as HPV. CHIS cancer data have been used in a wide range of research, often focusing on disparities in rates of cancer by race or ethnicity, gender, income, generation, citizenship status, and more.
Certainly, the challenge of finding providers varies by insurance status and the size of the available network. However, multiple other factors can complicate access, such as geography or language. While an obvious example of a barrier is an immigrant living in a rural area seeking a doctor that can speak Tagalog, it can be just as difficult for a woman in Los Angeles who depends on public transportation to find conveniently located breast cancer providers.