Menu - Public Hospital Redesign and Incentives in Medi-Cal (PRIME)
UCLA researchers evaluate statewide program aimed at promoting access to and improving the health of patients at public hospitals.
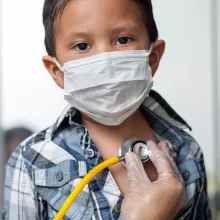
California has promoted value-based care in its public hospitals under a Medi-Cal 2020 Section 1115 Waiver called Public Hospital Redesign and Incentives in Medi-Cal (PRIME), a waiver overseen by California’s Department of Health Care Services (DHCS). A $3.7 billion demonstration project aimed at improving the health of Medi-Cal patients at public, municipal, and district hospitals, PRIME required public hospitals to significantly transform their outpatient care delivery to receive payment for improved performance.
Fifty-four public hospitals in California — including 17 designated public hospitals (DPHs) and 35 district and municipal hospitals (DMPHs) — implemented PRIME to achieve five overarching goals designed to improve care delivery, cultural competence, and patient health outcomes, as well as to move public hospitals towards value-based care.
The UCLA Center for Health Policy Research (CHPR) received a five-year grant from DHCS to evaluate the PRIME program. Nadereh Pourat, PhD, associate director at UCLA CHPR and director the Health Economics and Evaluation Research (HEER) Program, led a team of researchers who evaluated the PRIME program, conducting a mixed-method evaluation using a wide range of data sources including Medi-Cal enrollment, encounter, and claims data; hospital-reported metrics and narratives; and hospital surveys and semi-structured interviews, to assess the impact and highlight lessons learned through the program.
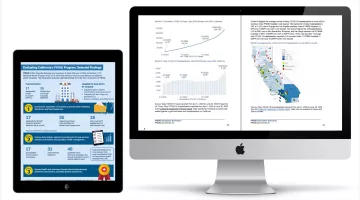
PRIME at a Glance
2.33
fewer hospitalizations per 1,000 patients per year among DPHs
6.32 and 15.36
fewer emergency department visits per 1,000 patients per year among DPHs and DMPHs, respectively
$836–$865
reduced Medi-Cal payments per patient per year at DMPHs and DPHs
In the initial Interim Evaluation of PRIME report, Pourat and the research team evaluated the PRIME program (i.e., following evidence-based guidelines), promoting better care outcomes (i.e., offering increased screening for cancer and tobacco use), and tracking better health (i.e., improvement of hypertension and diabetes control).
In the subsequent Preliminary Summative Evaluation of PRIME report, Pourat and team evaluated PRIME metric progression, challenges and successes, and plans for sustainability at the end of PRIME implementation.
The Final Summative Evaluation of PRIME report, the third and final report, showed that PRIME hospitals:
- Reduced hospitalizations (2.33 fewer per 1,000 patients per year among DPHs) and emergency department visits (6.32 fewer per 1,000 patients per year among DPHs; 15.36 fewer per 1,000 patients per year among DMPHs) for PRIME patients compared with patients of other providers.
- Reduced Medi-Cal payments per patient per year ($836 less among DMPHs; $865 less among DPHs).
- Used innovative approaches and modifications to implement PRIME projects, mitigating COVID-19 pandemic disruptions.
- Improved public hospitals’ ability to participate in managed care value-based payments.
The report was approved by the Centers for Medicare & Medicaid Services (CMS) in March 2023.
The findings of this evaluation highlight the importance of federal funding for initiating and promoting progress in quality improvement projects and can be used to inform federal and state Medicaid policies to promote better care, better health, and lower costs.