Californians in some areas less likely to benefit from policies curbing tobacco use
Areas with weak local regulations leave some communities more vulnerable to harm from tobacco use
Media Contact:
Mike Fricano
310-794-5553
Correction: This page was updated on March 20, 2024, to clarify the language in the first "key takeaway" describing who was least likely to be protected by tobacco-control policies.
Key takeaways:
- Populations in neighborhoods with low socioeconomic status were least likely to be protected by tobacco control policies in 2014–2019. Socioeconomic status considers education level, linguistic isolation, poverty, unemployment, and housing.
- 12.5% of California adults reported smoking during the last 30 days in places without local or state tobacco policies prior to the 2017 cigarette tax increase. The rate dropped to 7.7% in areas where both state and local policies were in place.
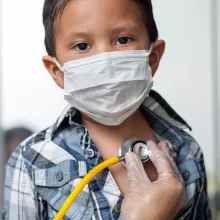
Although California has made progress reducing cigarette smoking rates during the past three decades, progress across communities in the state has been uneven, according to a policy brief from the UCLA Center for Health Policy Research (CHPR).
In what was one of the first studies to examine the impact of state and local policies on smoking behaviors, researchers found that cities with strong regulations limiting tobacco have greater reductions in adult cigarette smoking rates than cities with weak regulations or those that don’t have them. Strong local policies were also associated with decreased smoking rates among adult populations disproportionately harmed by the tobacco epidemic, thereby reducing health disparities resulting from cigarette smoking.
Those who have been disproportionately harmed include racial, ethnic, and sexual minorities; low-income, rural, or multiunit housing residents; and residents in neighborhoods with high concentrations of low-income populations or minoritized populations. Cigarette smoking remains the leading cause of preventable death and disease in the United States and California.
“What we learned in our study of how tobacco regulations are linked with tobacco use rates, especially among more vulnerable populations in California, was troubling,” said Ying-Ying Meng, DrPH, lead author of the policy brief and director of research at the UCLA Center for Health Policy Research.
California has been at the forefront in adopting policies to decrease smoking and its harmful public health effects. In 1995, it was the first state in the country to ban indoor smoking in workplaces, including restaurants; bars and gaming establishments were added in 1998.
In April 2017, California sharply increased the taxes on a pack of cigarettes by $2 to $2.87 per pack. Before that (2014–16), 12.5% of California adults reported cigarette smoking when in areas without local or state tobacco-curbing policies. After the state policy took effect (2017–19), rates declined to 7.7% where both state and local policies were in place, compared to 11% in areas with no local policies to supplement state regulations.
“Though California has led the United States in policy efforts to curb smoking, work remains to be done so that everyone can benefit,” said Meng, who is also a researcher at the UCLA Fielding School of Public Health.
The brief, which uses data from the 2014–2019 California Health Interview Survey (CHIS), combined adult data and existing state-, county-, and city-level tobacco control policies and neighborhood-level data on social drivers of health.
Differences across California’s 58 counties and 482 incorporated cities have created a patchwork of regulations. For the purposes of the brief, the researchers used grades indicating the strength of local tobacco control policies in four categories that are assigned by the American Lung Association. These were smoke-free outdoor ordinances (including dining areas, recreational areas, and public events); restrictions on smoking in apartment buildings; tobacco retailer licensing requirements; and ordinances regulating emerging issues such as flavored tobacco products.
UCLA researchers found that among those with low family incomes, 67% were unprotected by a smoke-free housing policy and 65% were unprotected by a policy reducing sales of tobacco products. Among people who lived in rural areas, 53% were unprotected by a smoke-free outdoor air policy while 80% were unprotected by policies reducing sales of tobacco products.
Other statistics of note that show disparities among income levels and race and ethnicity:
- 25.1% of Latinos who lived in low socioeconomic status neighborhoods were unprotected by local tobacco control policies, compared with only 7% unprotected in high socioeconomic neighborhoods.
- 17.2% of Blacks or African Americans who lived in neighborhoods with low socioeconomic status were unprotected by local tobacco control policies, while only 8.5% were unprotected in high socioeconomic neighborhoods.
- For people earning less than 400% of the federal poverty level ($12,490 for an individual and $25,750 for a family of four) smoking rates climbed from 12.5% in areas with policy grades of A, B, or C to 14.2% in areas with policy grades of D or F.
- Smoking rates for American Indians and Alaska Natives, and people who identified as two or more races were 14.4% for people living in places where the overall tobacco policy was graded A, B, or C, and they were 19.3% for people living in places with grades of D or F.
Meng said the brief provides a first-of-its-kind examination into inequities in tobacco control policy protection across adult priority populations and what effect these policies have on smoking behaviors. Priority populations include but are not limited to racial and ethnic minorities, LGBTQ people, people with low socioeconomic status, rural residents, current smokers, and school-age youth. Those surveyed said that enforcement of existing regulations was inconsistent.
“To eliminate disparities, it is critical to empower members of the communities who have been most harmed by the patchwork of regulations by providing resources, information, and partnership,” Meng said.
Read the publications:
- Policy Brief: State and Local Tobacco Control Policies Are Associated with Decreasing Cigarette Smoking Rates and Disparities
- Infographic
#
About the UCLA Center for Health Policy Research
The UCLA Center for Health Policy Research (CHPR) is one of the nation’s leading health policy research centers and the premier source of health policy information for California. UCLA CHPR improves the public’s health through high quality, objective, and evidence-based research and data that informs effective policymaking. UCLA CHPR is the home of the California Health Interview Survey (CHIS) and is part of the UCLA Fielding School of Public Health.