UCLA study suggests looking beyond area vulnerability indicators to identify at-risk populations
Researchers propose that using models may help find the most high-risk groups for pandemic relief and other vital resources
Media Contact:
UCLA CHPR Communications Team
Current data suggests that small ethnic populations in California ─ American Indians and Pacific Islanders, Cambodians, Filipinos, and Koreans ─ may have higher than average COVID-19 infection and death rates, but how can policymakers identify where to allocate needed resources, such as vaccines?
Using a combination of measures created by public agencies and UCLA can help guide efforts to identify at-risk groups for emergency conditions such as the pandemic, according to two new research reports by the UCLA Center for Neighborhood Knowledge, UCLA Center for Health Policy Research, and Ong & Associates.
The latest report, Vulnerability Indicators and At-Risk Smaller Populations in California and Los Angeles: American Indians, Pacific Islanders, and Select Asian Ethnic Groups, which was released today, takes a closer look at the performance of vulnerability indicators to spot high-risk smaller populations in California and Los Angeles County.
“It would be great to pinpoint for state and local policymakers where the vaccines should go to help these vulnerable populations,” said Paul Ong, PhD, director of the UCLA Center for Neighborhood Knowledge and co-lead author of a new study that analyzed where at-risk populations live. “Unfortunately, it's not that easy, because they are a hidden diaspora and not tied to a geographic place.”
The study, supported by a grant from the Robert Wood Johnson Foundation through the center for health policy research’s National Network of Health Surveys, looks at factors such as poverty and pandemic-related job risks among these racial and ethnic groups compared across various census tracts that are identified as the most high-risk areas in California and LA County. Three pre-pandemic indicators, built by the Centers for Disease Control and Prevention, Health Resources and Services Administration, and the Public Health Alliance of Southern California are used.
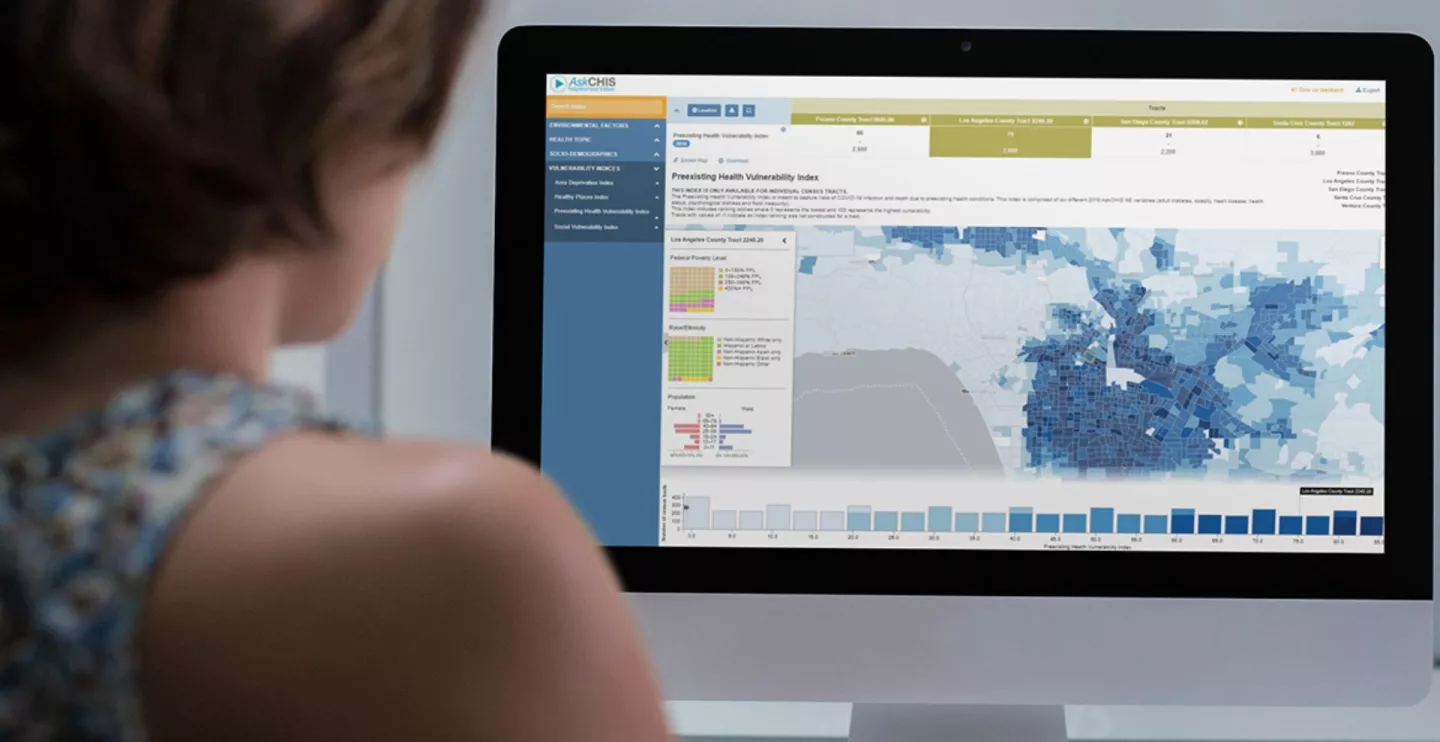
The UCLA Pre-Existing Health Vulnerability (PHV) index, based on data from the California Health Interview Survey (CHIS) and created with the UCLA BRITE Center for Science, Research and Policy, led by Vickie Mays, PhD, to capture risks of COVID-19 infection and death due to pre-existing health conditions, was also used by the researchers to look at simulations that indicate which racial and ethnic groups in vulnerable state and county areas may be most in need of services such as health care and other resources. This index is made up of six different 2016 AskCHIS Neighborhood Edition™ variables ─ adult diabetes, obesity, heart disease, health status, psychological distress, and food insecurity, and is currently being used by practitioners at UCLA Health.
“The data we’ve been compiling show that Pacific Islander and other smaller Asian groups are two to three times more likely than non-Latinx white workers to be essential workers, who are at a higher risk of being exposed during a pandemic. But they have received less attention because their numbers are fewer, which is why we are promoting more ways to use data to address striking disparities,” said Ninez Ponce, PhD, director of the UCLA Center for Health Policy Research and CHIS principal investigator.
Percentage scores in the simulation models show which rates of the overall population live in high-risk census tracts and what part of the population is captured as high-risk across each vulnerability indicator. The data show that 25% of all California and Los Angeles County residents live in highly vulnerable census tracts. As in the previous report, the findings note that there are limitations in each indicator in getting at underlying racial disparities and social and economic vulnerabilities. For example, one indicator may capture a certain racial and ethnic group at a higher rate due to high poverty rates or other representative data on state and county levels.
With the exception of the American Indian group, the smaller racial groups were found to be underrepresented in the riskiest areas that the four indexes identified. When researchers separated Asian American groups into three ethnicities ─ Cambodians, Filipinos, and Koreans ─ only Cambodian residents were identified as having a higher percentage of residents in vulnerable areas.
“While each tool was good at identifying a specific need, such as post-disaster help or help with hunger, together they failed to clarify where the small vulnerable groups live and how we can more accurately deliver them needed resources,” Ong said. “We need to look at more than just geographic factors, and other measures such as multigenerational housing, disability status, and occupation, that get at the social and economic factors related to health in order to address specific pandemic-related goals and relief efforts should be considered.”
Report authors emphasize that these measurement tools can be used as a starting point for policymakers, researchers, and other community stakeholders, and can be finetuned to identify which groups and places are considered vulnerable, as it shows the strengths and weaknesses of each indicator by looking at the potential gap in needs and services across these delicate racial lines.
Read the Publication:
#
The UCLA Center for Health Policy Research (CHPR) is one of the nation’s leading health policy research centers and the premier source of health policy information for California. UCLA CHPR improves the public’s health through high quality, objective, and evidence-based research and data that informs effective policymaking. UCLA CHPR is the home of the California Health Interview Survey (CHIS) and is part of the UCLA Fielding School of Public Health.
The UCLA Center for Neighborhood Knowledge is dedicated to translating its research to inform actionable neighborhood-related policies and programs that contribute to positive social change. We specialize in empirical spatial analysis and emphasizes the study of diversity, differences, and disparities among neighborhoods, and explicitly cover immigrant enclaves, low-income neighborhoods and minority communities.