Menu - Health Equity Program
Health equity means that everyone — regardless of their background or circumstances — has a fair opportunity to reach their full health potential. The UCLA Center for Health Policy Research (CHPR) is committed to providing research and data on the health and health care needs of marginalized communities.
A person’s race, ethnicity, sexual orientation, gender identity, gender, age, citizenship status, English proficiency, disability, and socioeconomic status, as well as social determinants of health — the conditions in which people are born, grow, live, work, and age — impact access to and quality of care, and influence health outcomes. UCLA CHPR’s Health Equity Program helps policymakers, advocates, researchers, community leaders, media, and other key stakeholders understand where health gaps exist.
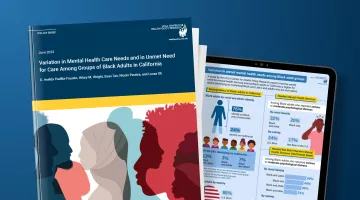
Led by Kathryn G. Kietzman, PhD, senior research scientist and Health Equity Program director, the Health Equity Program is recognized for its in-depth analysis, research, and technical assistance on the health issues and concerns of older adults, immigrants, sexual and gender minority groups, and racial and ethnic minority populations, such as American Indians and Alaska Natives.
Some of the Health Equity Program’s recent projects include:
Health Equity at a Glance
2 in 3
Latino and Asian immigrants in California perceive that immigrants who use government benefits such as income assistance, health care, food programs, and housing aid, would be prevented from gaining legal U.S. immigration status (Source: 2018, 2019 and 2020 California Health Interview Surveys/RIGHTS Study)
2 in 5
older adults and adults with disabilities in California reported that they had cut down on the amount they spent on food and/or saving for retirement (Source: 2019–2020 California Health Interview Survey/LTSS Study)
47.3%
of Latino and Asian immigrants who had ever been undocumented said they settled for a job that paid less than what they deserved and 28.1% did not get paid for hours worked (Source: 2018, 2019 and 2020 California Health Interview Surveys/RIGHTS Study)